I thought I would write about our walk with Cancer, not only to share our experiences, but just to write it all down so we can look back and have it in our “scrapbook”, if you will.
Thursday June 8th of 2017, I went to visit my primary care physician. I had denied and ignored the swelling in my right testicle for a number of months, and it was clear that something was not right. I realized that despite my dread and fear of visiting the doctor, it was time for me to go. After meeting with the doctor, he was unsure of the issue and scheduled a diagnostic ultrasound for the following week, Monday June 12th.
The following Monday, June 12th, I showed up for my ultrasound. After the technician did the scanning and imaging, she (yes it was a woman imaging my private parts) said she needed to have the doctor on staff take a look. A couple minutes later the doctor from radiology explains that they cannot get a good look into the testicle because the the tissue surrounding it was so dense. He then added that 9/10 times when they see something like this, it is cancer.
What?! Cancer? What just happened here? This is why I never go to the doctor because they find things wrong with you. Unfortunately, I couldn’t deny that there was something wrong, and I would need to simply face this head-on until I really knew what was going on.
An appointment was scheduled for the next day, Tuesday June 13th, with the urologist to get a better understanding of what was going on, and more importantly, what was going to happen next. Karen and I went to the appointment together, where we were told that this was a tumor, likely cancerous, but until they did some blood testing, imaging, and surgery to remove the testicle, we really wouldn’t know specifically what treatment would involve. This was a lot to take in, and seemed like even more ahead of us. Again, all I could do was put my head down, and focus on what was next. For now, that was chest x-rays, CT scan, and a full blood-work.
An orchiectomy, fancy name for the surgical removal of the testicle, was scheduled for next Thursday, June 22nd. Chest x-rays and CT scan showed a single lymph node in my abdominal area that was also enlarged, 4.5cm. Blood-work also showed elevated AFP (Alfa-Fetoprotein) markers, which indicate the presence of cancerous tumor as well. So, at this point is was pretty official, I had cancer. The only thing we really didn’t know yet was what specific type. We knew it was testicular cancer, but there are a few strains and until they did a pathology on the testicle/tumor, we wouldn’t know exactly what it was. They don’t do a biopsy of the testicle without removing it due to the risk of spreading cancer cells, the standard protocol is simply the orchiectomy.
So the surgery goes well, basically a couple hours, at Providence Newberg Hospital, and I am home that afternoon. Recovery should be 2-3 weeks, but the real concern is what are the results from the pathology. It seemed like it took forever, add into the calendar the July 4th holiday, and it wasn’t until July 18th that we had the follow-up appointment to go over the pathology results.
This is where we were confirmed that it was a mixed germ cell cancer of the following type: 55% yolk sac tumor, 25% teratoma, 15% seminoma and 5% embryonal carcinoma. This mixed germ cell cancer would in fact require chemotherapy, and possibly more surgery afterwards to address the lymph node in my abdomen. The next step is a meeting with an oncologist to develop and treatment plan. This is where things really started to sink in, that we are going to have to be treated for cancer.
The next step was scheduled chemotherapy, which would begin August 14th. The oncologist felt 3 rounds of BEP chemotherapy would be the most successful protocol, and given my age and health I would tolerate it well. BEP are the drugs used to treat testicular cancer, Bleomycin, Etoposide and Platinol, also called Cisplatin. Each round would be 3-weeks long; one full week with treatment each day, following by two more weeks receiving treatment only one day/week.
August 3rd I had a cardio pulmonary fitness test, to make sure I was a good candidate for the BEP therapy. It can cause issues in people with compromised respiratory systems, so I had to get approved first. I passed, and could proceed.
On August 7th, I received an IV access port in order to make the delivery of the drugs easier. The port was a receptacle placed in my chest, with a catheter leading to a vein in my chest/abdomen area. This was great, it allowed the nurses to plug in the IV directly into this port each time without ever having to hunt and search for a vein. The installation procedure was surgical, at the hospital, but I was in/out within a few hours.

Monday August 14th was my first day of chemotherapy. Thank goodness we have a nice local hospital close by with a cancer facility. Each day was an easy 12 minute drive. I sat in the lazy-boy recliner with my computer, typically for about 4 hours, while the drugs were delivered via IV through my port. Chemotherapy was much more tolerable than I expected. Towards the end of the first week I found myself getting more tired, but by the following week was already getting some energy back. Weeks 2 and 3 seemed pretty good overall, no severe fatigue or sickness.
I did however start to lose my hair the last week in August, and the following week decided to OWN IT and shaved it off. The first few days were very awkward, but within a week or two I found it quite comfortable and there was a sense of confidence just accepting that this is me, I am sick right now, and I am going to fight it head on.

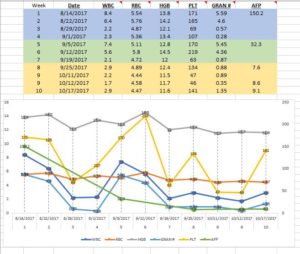
During the second round of chemo, which started September 4th, my body was getting more tired, and the chemo was having a cumulative effect on me. My white and red blood cells, as well as the platelet counts had bounced back after their big drop in week 3 of round 1, but they didn’t rebound to the normal levels prior to treatment. I was starting off round 2 more compromised that I was when I started round 1.
During the process I kept a spreadsheet of all of my blood counts, and always asked for the report from the nurses after each weekly blood draw. It was quite interesting to see how predictable the cycle was. Each week during chemo, all my counts would drop each week, almost to zero. But when it was time to start the next round, they were bouncing back. This was so cool to see how well the doctors understand the role of the medicine (poison), and the bodies natural cycle and the time it needs to fight back.
Round 3 was, as expected, the hardest of them all. I was very tired all the time, taking lots of naps, losing weight, not sleeping well. It was pretty rough there towards the end. Here is one of the many places around our farm where I would just sit and rest, usually with our therapy goats! Breathing fresh air, sitting in the shade, having my goats hang out close by was such an important part of getting through this.
My blood counts were really in the tank, and I had to be careful about germs and wounds because my immune function and blood clotting abilities were highly compromised. But, during the whole process I did not experience any nausea at all. What a blessing!
Before you knew it, October 11th, 2017 was here, and I was going in for my last chemo treatment. It was a little emotional as I said a big THANK YOU to my wonderful nurses Dawn and Sandy who had taken such good care of me over the last 9 weeks. It was really a shock that we were all done, it had gone by very fast!
October 12th was a final CT scan to take a look and make sure there was nothing else to be concerned with. October 17th, met with the oncologist to discuss the results, where he informed me the lymph node had shrunk from 4.5cm to 1cm. Awesome news! Bad news was the oncologist still wanted to test it, so he wanted to do a robotically-assisted laparoscopic biopsy. OK, no big deal.
Then, on October 31st I met with the surgeon, who changed up the plan. He wanted to avoid the laparoscopic biopsy, because IF they found it was cancerous, we would have to go back in again, and the scar tissue would make that follow-up surgery much more difficult. His plan was to be aggressive, and perform an RPLND, a pretty extensive surgery where he would remove a network of lymph nodes in my abdominal area. This would almost guarantee a high cure rate as it would remove any doubt there would be no remaining cancer. Again, head down and move forward and fight this thing.
Surgery was at Legacy Good Samaritan Medical Center, November 15th. Legacy Good Sam is what they call a high volume surgery center, another reminder of just how large this surgery was going to be, they only perform it in a handful of facilities. I was in surgery for around 6 hours, and everything went well and as planned. I have an awesome 10.5″ vertical scar on my abdomen as a souvenir. Spent 2 nights in the hospital and my wonderful wife drove me home on Friday. Boy, was I sore and why did I agree to this surgery??!!
Now to wait for the pathology results. Doc said it would be just a few days. Tick-tock, tick-tock. I finally called his office the following Wednesday to check in and was informed that “we show those results are in but have not been reviewed by the doctor. He is off the rest of the week for Thanksgiving.” What??!! More waiting I guess?? I would just have to continue my rest/recovery/waiting through the long holiday weekend and wait for results next week.
The phone rings Thanksgiving morning, and it is the doctor. I can hear voices, children, people talking and laughing, these are obviously his friends and family in the background on this Thanksgiving morning. He tells me that the tissue they removed during the surgery was necrotic tissue. Basically dead tissue, some of which had been cancerous but the chemo did the job and it was dead. I was in remission. WOW, I had spent the last 5 months of my life hoping and praying to get to this point, I don’t think I could have been more relieved. I gave him a big THANKS for calling on the holiday, it was a truly thoughtful act on his part. He replied that he doesn’t always get to share good news, so it was a good phone call for him too. They have a harder job than we can imagine.
I would spend the next weeks recovering from surgery, going to follow-up appointments, having my port removed, and getting back to normal life. Trying to gain my strength back. Trying to pick up where we were all forced to leave things just a few short months ago.
It is a new normal now though, as you see things a little different. There is always a fear anytime I feel a strange ache or pain. Side effects, while minimal will always remind me of the damage cancer, and it’s necessary treatment, can cause.
I am grateful for my family who picked up all my slack during this process. I am thankful for the wonderful medical community who made me as comfortable as possible during this process. I am thankful for my employer who allowed me to continue to work and supported me thoughout. And I am most thankful to God our creator who makes all things possible.
If you actually read through this whole page, thank you! I know it was long, but didn’t know what to cut out.
From the farm, cancer free,
Michael